Table of Contents
Subtitle: How a stray PDF of the Beck Depression Inventory led me from the isolating fog of depression to the clarity of a conversation, and what it reveals about the power and peril of a revolutionary psychological tool.
The Unnamable Weight
It began not as a sharp pain, but as a dull, pervasive weight.
It was a fog that settled over everything, muting the colors of a world that I knew, intellectually, was still vibrant.
I could laugh with friends at dinner, my face performing the correct sequence of muscle contractions, while inside I felt a “gut wrenching loneliness”.1
I could be in a room full of people I loved, yet feel “completely disconnected”.2
Depression, I would later learn, is a master of disguise; it shows itself differently for everyone, making it a profoundly solitary and incommunicable experience.1
My own experience was a paradox of feeling everything and nothing at once.
There was the constant, low-grade anxiety, a hum of dread beneath the surface of everyday life.
And then there was its counterpart: a profound numbness, a checking out from my own existence where I felt “literally nothing”.1
I struggled to give this state a name.
It wasn’t simple sadness, which usually has a cause you can point to.
This was a formless, causeless ache, a sense of “complete solitude” that felt both internal and infinite.1
My brain, my own internal narrator, had turned against me, whispering that I was unlovable, unwanted, and, most damningly, that no one could possibly understand.1
I felt as though I were “stuck in thick, oily goo,” where every step toward the light only made the mire stickier and darker.3
This inability to articulate my own suffering was the cruelest part of the affliction.
How can you ask for help when you don’t have the words for what’s wrong? How do you build a bridge to another person when you can’t even map your own side of the chasm? This internal chaos led me, as it leads millions, to the cold, blue light of a screen in the dead of night.
My search history became a litany of desperation: “symptoms of chronic unhappiness,” “why do I feel numb,” “do I have depression.” It is a uniquely modern ritual; studies show that roughly one in three American adults have turned to the internet to diagnose a health issue.4
I was presenting as “normal” to the outside world, holding down a job, meeting obligations, but my internal life was crumbling.5
My digital quest first led me into a bewildering carnival of online “depression quizzes.” They were everywhere, promising instant insight with a few clicks.
These tests, I now know, are often clinically worthless, more akin to a social media personality quiz than a valid psychological tool.6
They frequently conflate serious clinical diagnoses with personality quirks, labeling someone who enjoys tidy spaces as “obsessive-compulsive” or someone who dislikes being alone as “borderline”.7
The quizzes were short, often filled with jokes, and utterly opaque about their methods.7
Each one I took left me feeling more frustrated and alone.
The results were either so generic as to be meaningless or so extreme that I dismissed them, feeding the narrative that I was simply “making it up.” This journey through the internet’s unregulated wilderness of self-diagnosis is fraught with peril.
It can lead one to misinterpret normal life struggles as chronic disorders, to ignore critical symptoms that don’t fit a quiz’s narrow framework, or even to develop a kind of “cyberchondria,” a state of escalating health anxiety fueled by the very search for answers.4
The experience underscored a profound truth about my struggle.
My search for a test, for a “PDF,” was not just a hunt for information.
It was a desperate search for a language.
The amorphous, ineffable nature of my suffering was its defining feature; it was a monster without a shape.
Personal accounts of depression are filled with this struggle for articulation: “I don’t really know how to explain this numbness” 1; “I didn’t understand what was going on”.2
This lack of vocabulary creates a deep chasm of isolation, a conviction that “no one will ever truly understand who I am”.1
Humans have a fundamental need to categorize and label their experiences to make them real, to make them manageable.
An objective, structured tool—something like a questionnaire—promised a pre-fabricated vocabulary for my chaos.
The term “PDF” itself held a certain allure; it suggested something official, concrete, and stable, a stark contrast to the shapeless fog in my mind.
I wasn’t just looking for a score; I was looking for a script.
A Glimmer in the Fog: The Beck Depression Inventory
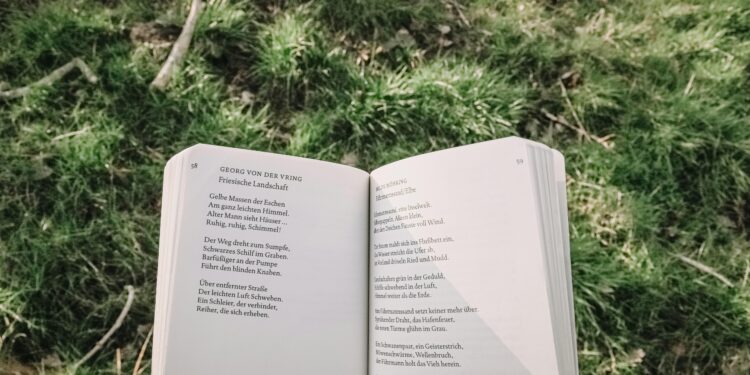
After wading through the digital swamp of clickbait quizzes, I stumbled upon something different.
It was a clean, professional-looking document, a PDF file simply titled “Beck Depression Inventory-II.” There were no cartoon sad faces, no promises of a five-minute fix.
There were just 21 questions.
As I began to read, a strange and unsettling feeling washed over me: recognition.
These questions were not the blunt instruments I had encountered before.
They were specific, nuanced, and uncomfortably precise.
They felt as if someone had been listening to the secret, circular monologues in my head and transcribed them.
- “I feel the future is hopeless and that things cannot improve.” 9
- “I have lost all of my interest in other people.” 9
- “I have to push myself very hard to do anything.” 9
- “I am so sad or unhappy that I can’t stand it.” 10
- “I am too tired to do anything.” 9
Each item presented a set of four statements, ranked by severity.
I had to choose the one that best described how I had been feeling over the “past two weeks, including today”.11
The process was methodical.
I went through all 21 items, circling the number—from 0 to 3—that corresponded to my chosen statement.
At the end, I followed the simple instruction: add up the numbers.
The maximum possible score was 63.12
My total was 32.
I scrolled down the PDF and found the scoring key.
It was a simple chart that translated the number into a level of severity.
0-13: Minimal depression.
14-19: Mild depression.
20-28: Moderate depression.
29-63: Severe depression.14
Thirty-two.
Severe depression.
The word hung there on the screen, stark and absolute.
It wasn’t a diagnosis—the document itself cautioned against that—but it was a data point.
It was the first piece of external, objective evidence that the weight I had been carrying was real.
For months, perhaps years, I had been engaged in a silent debate with myself: Am I really suffering, or am I just weak? Am I sick, or am I just complaining? Is this real, or am I making it all up? The number 32 was an answer.
It was a validation that cut through the fog of self-doubt.
It was a snapshot of my mental state, a confirmation that what I was experiencing was a recognized and measurable phenomenon.18
It mirrored the experience of so many who turn to these tools for a sign that their illness is real, not a personal failing.20
Looking back, I realize that the therapeutic power of the Beck Depression Inventory began the moment I started answering its questions.
The very structure of the test is a form of cognitive intervention.
My depression had felt like a monolithic, unnamable beast.
But the BDI doesn’t ask, “Are you overwhelmed by a terrifying monster?” Instead, it breaks that monster down into 21 distinct, observable parts: Sadness, Pessimism, Past Failure, Loss of Pleasure, Self-Dislike, and so on.9
It forces you to differentiate, to grade your own experience on a scale of 0 to 3.
Am I just “less interested in other people than I used to be” (a 1), or have I “lost all of my interest in other people” (a 3)?.9
This process of deconstruction is a foundational element of cognitive therapy.
It takes an overwhelming, abstract concept and renders it concrete, observable, and manageable.
The act of taking the test was, in itself, the first step in learning to observe my own thoughts and feelings from a distance.
It was a form of proto-therapy, delivered through a simple PDF.
The Architect of Understanding: Aaron T. Beck and the Cognitive Revolution
Armed with a name—”Beck”—and a number—”32″—my search changed.
I was no longer casting a wide, desperate Net. I was investigating a lead.
Who was this Beck? And how did he create a list of questions that seemed to know me better than I knew myself? My research led me to the story of Dr. Aaron T.
Beck, a man who lived to be 100 years old (1921-2021) and who is now widely regarded as the father of cognitive therapy and cognitive behavioral therapy (CBT).23
His story, I discovered, was one of scientific courage and a revolutionary departure from the psychiatric orthodoxy of his time.
When Beck began his career in the 1950s, the world of psychiatry was dominated by Freudian psychoanalysis.25
The prevailing theory held that depression was a psychic malady caused by “inverted hostility against the self”.25
In this model, a person’s anger, unable to be expressed outwardly, turns inward, leading to self-reproach, guilt, and a masochistic “need to suffer”.26
Beck, trained in this tradition, set out to conduct experiments he fully expected would validate these core psychoanalytic precepts.24
But his research led him to a startling conclusion: the theory was wrong.
Instead of finding evidence of inverted hostility, Beck found something else entirely when he simply listened to his patients.
By collating their “verbatim descriptions of their symptoms,” he noticed that their conscious, spoken thoughts were not centered on anger, but on themes of loss, defeat, and rejection.23
He discovered that his depressed patients were plagued by a constant stream of negative thoughts that seemed to arise spontaneously.
He famously termed these “automatic thoughts”.23
This was the epiphany that would change modern psychology.
Beck realized that it wasn’t some deep, inaccessible unconscious drive causing the depression.
The cause was right there on the surface, in the patient’s own cognitions.
He identified that these automatic thoughts consistently fell into three distinct categories, a framework he called the cognitive triad:
- Negative ideas about the self (e.g., “I am worthless,” “I am a failure”).
- Negative ideas about the world (e.g., “The world is a cruel place,” “No one cares about me”).
- Negative ideas about the future (e.g., “Things will never get better,” “My future is hopeless”).23
This framework provided a radical new way of conceptualizing depression.
The prevailing view was that distorted thinking was a symptom of the mood disorder.
Beck proposed the opposite: the sustained, inaccurate, and intrusive negative thoughts were the cause of the depression.25
From this revolutionary theory, the Beck Depression Inventory was born in 1961.
It was a tool designed specifically to provide a quantitative measure of depression’s intensity by assessing the very cognitions Beck had identified.25
Its structure was a direct reflection of his cognitive triad.
An item like “I blame myself for everything bad that happens” probes the self.
An item like “I have lost all of my interest in other people” probes the world.
And an item like “I feel discouraged about the future” probes the future.25
The creation of the BDI was more than the development of a new tool; it was the physical manifestation of a paradigm shift.
It moved the locus of depression from the therapist’s interpretation of a patient’s unconscious to the patient’s own self-reported thoughts.12
This shift represented a profound act of empowerment, fundamentally altering the power dynamic in therapy.
The psychoanalytic model positioned the therapist as the expert interpreter, the sole holder of the keys to the patient’s hidden psyche.
The patient’s own words were merely clues, symbols to be deciphered.
Beck’s approach inverted this.
By building an entire theory and its primary measurement tool on the “verbatim descriptions” of patients, he made a powerful statement: the individual’s subjective experience is the most valid source of data about their own suffering.
The development of a self-report inventory placed the instrument of measurement directly into the hands of the patient.
It was a declaration that said, “You are the expert on your own experience.
Your perception is the primary data.
You can measure this.” This philosophical pivot, which prefigured the modern emphasis on patient-centered care, was arguably as important as the tool’s scientific utility.
The Blueprint of the Mind: Deconstructing the BDI-II
My initial encounter with the BDI-II was purely emotional—a jolt of recognition and validation.
But my intellectual curiosity, sparked by the story of Aaron Beck, pushed me deeper.
I wanted to understand the instrument itself.
What made these 21 questions so different from the thousands of others online? I learned that the BDI-II I had found was the result of decades of refinement, a clinical instrument honed by science.
Evolution to a Modern Standard
The BDI-II, published in 1996, is the third major version of the scale, following the original BDI in 1961 and a minor revision, the BDI-1A, in 1978.25
The most significant changes were made to align the inventory with the diagnostic criteria for Major Depressive Disorder as laid out in the
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), the clinical bible of psychiatry at the time.13
This was not a cosmetic update.
Researchers had found that some items on the original scale, such as those concerning weight loss, body image, and somatic preoccupation, were less effective at assessing depression, particularly in outpatients who were being treated earlier in their illness than in the 1960s.11
To increase the tool’s sensitivity and diagnostic relevance, four items were replaced with questions about
Agitation, Worthlessness, Concentration Difficulty, and Loss of Energy.11
Furthermore, all but three of the original items were reworded for clarity, and the timeframe for assessment was changed from “the past week” to “the past two weeks, including today,” to match the DSM’s definition of a major depressive episode.11
Anatomy of the 21 Questions
These 21 items are not a random collection of sad thoughts.
They are a systematic and comprehensive probe into the core components of the depressive experience.
Clinicians and researchers typically group the BDI-II items into several clusters that cover the full spectrum of the disorder.13
| Symptom Cluster | Description | Sample BDI-II Item Statement (Highest Severity) |
| Cognitive | Thoughts about self, world, and future. | “I feel the future is hopeless and that things cannot improve.” (Pessimism) |
| “I feel I am a complete failure as a person.” (Past Failure) | ||
| “I blame myself for everything bad that happens.” (Self-Dislike) | ||
| Affective | Emotional states and feelings. | “I am so sad or unhappy that I can’t stand it.” (Sadness) |
| “I am dissatisfied or bored with everything.” (Loss of Pleasure) | ||
| “I would kill myself if I had the chance.” (Suicidal Thoughts) | ||
| Somatic/Vegetative | Physical and bodily experiences. | “I am too tired to do anything.” (Tiredness or Fatigue) |
| “I wake up several hours earlier than I used to and cannot get back to sleep.” (Changes in Sleep) | ||
| “I have no appetite at all anymore.” (Changes in Appetite) |
This structure reveals the tool’s sophistication.
It moves beyond a simple inquiry into mood to systematically assess the cognitive distortions, emotional pain, and profound physical toll that characterize clinical depression.
The Science of a Good Test: What Makes the BDI-II Legitimate?
The critical difference between the BDI-II and a random online quiz lies in a field of study called psychometrics—the science of measuring mental faculties and processes.
For any scientific instrument to be considered useful, whether it’s a telescope or a psychological test, it must possess two key qualities: reliability (consistency) and validity (accuracy).
To understand this, it helps to use an analogy.
Think of a psychological test as a tool for measuring something invisible, like the temperature of a room.
Reliability is like a good thermometer’s consistency. If you place it in a room that is 72 degrees, you expect it to read 72 degrees every time you look.
If it reads 72, then 95, then 54, the thermometer is unreliable and therefore useless.
It lacks consistency.
The BDI-II demonstrates excellent reliability in two ways:
- Internal Consistency: This asks if all 21 questions are pulling in the same direction—if they are all measuring the same underlying concept (depression). The BDI-II has a very high internal consistency, with a statistical value known as Cronbach’s alpha of approximately 0.91 to 0.92.13 This indicates that the items are highly interrelated and cohesively measure the depressive syndrome.
- Test-Retest Reliability: This asks if the test gives stable results over a short period. The BDI-II has a remarkable one-week test-retest reliability correlation of r=0.93.11 This means that if a person takes the test one week and then again the next (without any major life event or treatment intervention), their scores will be extremely similar. This proves the BDI-II is not just measuring fleeting daily moods but a more stable underlying state.13
Validity is about the thermometer’s accuracy. A reliable but invalid thermometer might consistently read 85 degrees in our 72-degree room.
It’s consistent, but it’s consistently wrong.
Validity ensures that the instrument measures what it actually claims to measure—in this case, depression, and not some other related concept like anxiety or general distress.36
The BDI-II has demonstrated strong validity across multiple domains:
- Content Validity: The test’s questions comprehensively cover the construct of depression. As mentioned, the BDI-II was specifically revised to align with the official DSM-IV criteria, giving it strong content validity.13
- Concurrent and Convergent Validity: The BDI-II’s scores correlate highly with other established measures of depression. For example, its correlation with the Hamilton Depression Rating Scale, a clinician-administered gold standard, is high (r=0.71).11 It also converges well with newer scales like the Patient Health Questionnaire-9 (PHQ-9).31
- Discriminant Validity: Just as importantly, the BDI-II does not correlate highly with measures of different psychological constructs, such as anxiety.31 This shows it can discriminate between different types of psychological distress.
This scientific rigor is what elevates the BDI-II from a simple checklist to a trusted clinical and research instrument, used in over 7,000 studies and translated into dozens of languages.28
| Psychometric Property | Definition | BDI-II Finding | Source Snippet(s) |
| Internal Consistency | Do all the items measure the same construct? | Excellent (Cronbach’s α ≈.91-.92) | 13 |
| Test-Retest Reliability | Are scores stable over a short period? | Excellent (r ≈.93 over one week) | 11 |
| Content Validity | Do the items cover the full range of the construct? | High (Items align with DSM-IV criteria) | 11 |
| Concurrent/Convergent Validity | Do scores correlate with other depression measures? | High (e.g., r=0.71 with Hamilton Scale) | 11 |
| Factor Structure | What are the underlying dimensions? | Robust two-factor (Cognitive-Affective, Somatic-Vegetative) or three-factor models are common. | 35 |
The Conversation Starter: From a Score to a Solution
My score of 32 was a private revelation, a moment of clarity in the fog.
But a number, no matter how validating, is not a plan.
It’s a signpost, not a destination.
The most important journey was the one I took next: from the solitude of my computer screen to the shared space of a therapist’s office.
I remember the appointment vividly.
The usual anxieties of a first session were there, but this time, I had something new.
I had a piece of data.
Instead of struggling to find the words to describe the “unnamable weight,” I had a starting point.
“I’m here because I’ve been feeling…
off,” I began, my voice faltering.
“I actually took a test online.
The Beck Depression Inventory.
My score was 32.”
The therapist nodded, a look of understanding on her face.
And with that, the conversation began.
She explained that the BDI-II was more than just an intake form; it was a cornerstone of a modern, evidence-based approach called Measurement-Based Care (MBC).41
“Think of this score not as a final grade or a label,” she explained, “but as our starting point on a map.
Or, a better analogy might be a blood pressure cuff.
If you have high blood pressure, your doctor doesn’t just give you a pill and say, ‘See you in a year.’ They measure your blood pressure regularly to see if the treatment is working.
They track the data.
If it’s not improving, they adjust the plan—maybe a different dose, a new medication, or adding diet and exercise.
We’re going to do the exact same thing for your mental health”.44
This analogy was a revelation.
It reframed my understanding of therapy from a mysterious, purely conversational art to a collaborative, data-informed science.
MBC, she explained, is the practice of routinely collecting patient-reported outcomes—like my BDI-II score—to systematically track progress and guide treatment decisions in partnership with the patient.41
My score of 32 was our baseline.
She told me I would retake the BDI-II periodically, perhaps every four to six weeks, so we could objectively see if our work together was having an effect.14
This systematic tracking is crucial, as research shows that clinicians, relying on unstructured judgment alone, often struggle to accurately detect which patients are not improving or are even getting worse.41
The use of the BDI-II within this MBC framework transformed the therapeutic process.
It was no longer a passive experience where I simply talked and hoped for the best.
It became an active collaboration.
When my score dropped to 25, we could celebrate that progress and analyze what had worked.
“Your score on ‘Loss of Energy’ went down by two points,” she might say.
“What did you do differently these past few weeks that might have contributed to that?” When a score stagnated, it prompted a different conversation: “The numbers haven’t moved much.
What barriers are we hitting? Should we rethink our approach?”.14
This process fundamentally shifted my role from that of a passive recipient of care to an active participant in my own recovery.
I was no longer just describing my feelings; I was providing structured data that directly influenced my treatment plan.
This shared analysis of my own well-being demystified therapy and strengthened my connection with my therapist.
I felt heard and respected, because my own perspective, quantified and tracked over time, was a central driver of the process.
This increased engagement and collaboration, I later learned, is a key reason why MBC is associated with better patient outcomes, faster symptom reduction, and lower dropout rates from therapy.41
The BDI-II, which I first encountered as a tool for self-assessment, had found its true purpose: as a tool for communication and collaboration.
Reading the Fine Print: A Tool’s Power and Its Limits
As my journey continued, my understanding of the BDI-II matured.
The initial awe at its power was tempered by a more nuanced appreciation of its limitations.
Like any powerful tool, it is designed for a specific purpose and can be dangerous when misused.
The very PDF that had been my lifeline, I came to understand, was also a source of significant ethical concern.
A Screener, Not an Oracle
The most critical distinction my therapist helped me understand is that the BDI-II is a tool for measuring the severity of symptoms, not for providing a definitive diagnosis.16
A high score is a powerful indicator, a red flag that warrants a comprehensive clinical evaluation.
But it is not the evaluation itself.
A formal diagnosis of Major Depressive Disorder requires a skilled clinician to conduct a thorough interview, take a detailed history, and rule out other potential causes for the symptoms, such as other psychiatric conditions, underlying medical illnesses, or the effects of medication or substance use.14
My score of 32 meant I was very likely depressed, but it didn’t tell me why, or what other factors might be at play.
Known Limitations and Biases
Even within its intended use, the BDI-II is not infallible.
It has known limitations that require careful interpretation by a trained professional.
- The Subjectivity of Self-Report: The inventory’s greatest strength—that it captures the patient’s own perspective—is also a potential weakness. It relies entirely on an individual’s ability and willingness to report their symptoms accurately. Some people may consciously or unconsciously minimize their symptoms due to shame or stigma, while others might exaggerate them. This is known as self-report bias.30
- Somatic Symptom Overlap: For individuals with chronic medical conditions like cancer, heart disease, or chronic pain, the BDI-II can be tricky to interpret. Many symptoms of depression—fatigue, loss of energy, changes in sleep and appetite—are also symptoms of the physical illness itself.17 This overlap can lead to inflated scores and false-positive results for depression, requiring a clinician to carefully disentangle the sources of the symptoms.28
- Cultural Validity: Depression is a universal human experience, but its expression is not. While the BDI-II has been translated into over 90 languages and validated in numerous cultures, its accuracy is not uniform.25 Research shows significant cross-cultural differences in how depressive symptoms are reported. For instance, one study found that Finnish participants reported higher rates of irritability and sleep changes, while Mexican participants reported higher rates of self-criticalness and feelings of punishment.51 People from some Eastern cultures may be more likely to express depression through somatic (physical) symptoms, whereas Western cultures may emphasize cognitive (thought-based) symptoms.53 Furthermore, the original normative sample used to establish the BDI-II’s scoring cutoffs was predominantly White, which may limit its applicability to diverse populations.30 A responsible clinician must consider these cultural factors and may need to adjust their interpretation of the scores accordingly.14
The Ethics of the “Free PDF”
This brought me back to the document that started my journey.
I learned that the official BDI-II is not a free resource intended for public distribution.
It is a copyrighted clinical instrument published and sold by Pearson, a major educational and assessment company.13
The manual, scoring keys, and official forms must be purchased, a system designed to ensure the tool remains in the hands of trained professionals who understand its complexities and limitations.
The existence of my “free PDF” represents a significant ethical problem.
The unsupervised use of a powerful psychological assessment violates core ethical principles, such as those outlined in the Belmont Report, a foundational document for human subject research.57
The principle of “Respect for Persons” requires that individuals are treated as autonomous agents and that those with diminished autonomy are protected.
Handing someone a powerful psychological tool without the framework for informed consent, professional interpretation, and a clear follow-up protocol fails this standard.57
The risks are not theoretical.
A high rate of false positives means that many people who self-administer the test online may incorrectly label themselves as depressed, causing unnecessary anxiety and distress.58
More dangerously, the BDI-II contains an item on suicidal thoughts and wishes.
A high score on this item (“I would kill myself if I had the chance”) is a critical emergency signal that demands immediate safety planning by a professional.9
A static PDF file cannot intervene.
It cannot ask follow-up questions.
It cannot help.
This creates a paradox of access.
The very qualities that make the BDI-II such a good and respected instrument—its clarity, its ease of use, its quantifiable results—also make it dangerously appealing for misuse when ripped from its clinical context.
Its scientific success has fueled a public demand that has led to its unauthorized proliferation online, which in turn undermines the very safeguards designed to ensure it is used safely and effectively.
Finding a BDI-II online is like finding a surgeon’s scalpel on the street.
It is a precision instrument, sharp and effective in the right hands, but capable of causing serious harm when used without training and expertise.
Beyond the Score: Finding a Language for the Self
The Beck Depression Inventory did not cure me.
Therapy, human connection, medication, and a great deal of personal work did that.
But the BDI-II was the key.
It was the tool that unlocked the door to that treatment.
It gave my unnamable weight a name, my formless fog a structure, and my silent suffering a voice.
My recovery has been a journey from a single, terrifying number to a rich, complex, and ongoing narrative.
In the beginning, I was fixated on the score.
A 32 was a brand of severity.
A 25 was a sign of hope.
A 15 was a victory.
Over time, with the guidance of my therapist, I learned to see the score not as a judgment but as data.
It became a weather report for my internal climate—a useful, objective indicator of the current conditions, but not the whole of the landscape.
The greatest transformation, however, was not in the numbers, but in language.
Before the BDI, my pain was a monolithic, inarticulate weight.
After immersing myself in its world, I had a new vocabulary.
I could understand and describe my experience with a new precision.
I learned to differentiate between the cognitive distortions that fueled my pessimism, the affective states of sadness and irritability, and the somatic symptoms of fatigue that dragged me down.
I moved from a place of helpless confusion to one of informed self-awareness.
The BDI-II, born from Aaron Beck’s revolutionary act of listening to his patients, had taught me how to listen to myself.
My story began with a feeling of being fundamentally misunderstood, of living an experience so alien it could never be communicated.
It is a common feeling among those who suffer.
As one person wrote, “I can’t make anyone understand how it is for everyone, but I can tell you how it alters my life, and maybe that will help people understand”.1
If you see yourself in the “before” picture of this story—if you are lost in that same fog, struggling with that same weight—know that your struggle is real and valid.
And if your search leads you to a PDF of the Beck Depression Inventory, do not treat it as your destination.
See it for what it is: a signpost pointing you toward help.
The goal is not to get a score; the goal is to start a conversation.
The BDI-II is a remarkable map of the territory of depression, one of the most well-crafted we have.
But no one should have to navigate that territory alone.
Find a guide.
Works cited
- My Depression in My Life | NAMI: National Alliance on Mental Illness, accessed August 9, 2025, https://www.nami.org/Personal-Stories/My-Depression-in-My-Life
- Gabi’s story: my struggle with speaking up about my depression and loneliness, accessed August 9, 2025, https://www.mentalhealth.org.uk/explore-mental-health/stories/gabis-story-struggle-speaking-about-my-depression-and-loneliness
- Patient stories – Baycrest, accessed August 9, 2025, https://www.baycrest.org/baycrest/education-training/educational-resources/late-life-depression/understanding-late-life-depression/patient-stories
- Why Self-Diagnosing Mental Health Conditions Can Be Dangerous – BetterHelp, accessed August 9, 2025, https://www.betterhelp.com/advice/teenagers/why-you-shouldnt-self-diagnose-your-mental-health/
- Is there a good online test to see if you’re depressed? – Reddit, accessed August 9, 2025, https://www.reddit.com/r/depression/comments/7nuzhs/is_there_a_good_online_test_to_see_if_youre/
- How Accurate Are Mental Health Screenings Available Online? – Proem Health Blog, accessed August 9, 2025, https://blog.proemhealth.com/how-accurate-are-mental-health-screenings-available-online
- How Accurate Are Online Mental Health Tests? – GoodTherapy.org, accessed August 9, 2025, https://www.goodtherapy.org/blog/how-accurate-are-online-mental-health-tests-1005187
- The Dangers of Self-Diagnosing Your Mental Health – Nationwide Children’s Hospital, accessed August 9, 2025, https://www.nationwidechildrens.org/family-resources-education/700childrens/2024/03/the-dangers-of-self-diagnosing-your-mental-health
- Beck’s Depression Inventory, accessed August 9, 2025, https://www.ismanet.org/doctoryourspirit/pdfs/Beck-Depression-Inventory-BDI.pdf
- Beck Depression Inventory – Terappin, accessed August 9, 2025, https://terappin.com/en/test/beck-depression-inventory
- Beck Depression Inventory 2 | BDI-II | BDI 2 Manual Scoring, accessed August 9, 2025, https://www.bmdshapi.com/beck-depression-inventory-ii/
- Beck Depression Inventory (BDI) – Addiction Research Center, accessed August 9, 2025, https://arc.psych.wisc.edu/self-report/beck-depression-inventory-bdi/
- Beck Depression Inventory | Occupational Medicine – Oxford Academic, accessed August 9, 2025, https://academic.oup.com/occmed/article/66/2/174/2750566
- Beck Depression Inventory: A Clinical Tool for Measuring Depression Severity with Beck Depression Inventory – Blueprint, accessed August 9, 2025, https://www.blueprint.ai/blog/beck-depression-inventory-a-clinical-tool-for-measuring-depression-severity-with-beck-depression-inventory
- www.bmdshapi.com, accessed August 9, 2025, https://www.bmdshapi.com/beck-depression-inventory-ii/#:~:text=Thus%20BDI%2DII%20total%20scores,considered%20to%20be%20%E2%80%9CSevere.%E2%80%9D
- Beck Depression Inventory (BDI): Uses, Reliability, Where to Take the Test – Mentalyc, accessed August 9, 2025, https://www.mentalyc.com/blog/beck-depression-inventory
- Beck Depression Inventory-II (BDI-II) | NP Psych Navigator, accessed August 9, 2025, https://www.nppsychnavigator.com/Clinical-Tools/Psychiatric-Scales/Scale-1-(2)
- Take a Mental Health Test – MHA Screening, accessed August 9, 2025, https://screening.mhanational.org/screening-tools/
- “I Wanted to See How Bad it Was”: Online Self-screening as a Critical Transition Point Among Young Adults with Common Mental Health Conditions, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9075814/
- Does anyone else take the “Do You Have Depression” Quizzes online bc you already know the answer? – Reddit, accessed August 9, 2025, https://www.reddit.com/r/depression/comments/8aggum/does_anyone_else_take_the_do_you_have_depression/
- I feel pathetic for taking a depression quiz online. : r/depression_help – Reddit, accessed August 9, 2025, https://www.reddit.com/r/depression_help/comments/14g3mmn/i_feel_pathetic_for_taking_a_depression_quiz/
- Validity of self‐reporting depression in the Tabari cohort study population – PMC, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7722659/
- Aaron Beck – Wikipedia, accessed August 9, 2025, https://en.wikipedia.org/wiki/Aaron_Beck
- Aaron T. Beck, MD | Pearson Assessments US, accessed August 9, 2025, https://www.pearsonassessments.com/professional-assessments/products/authors/beck-aaron.html
- Beck Depression Inventory – Wikipedia, accessed August 9, 2025, https://en.wikipedia.org/wiki/Beck_Depression_Inventory
- Dr. Aaron T. Beck, accessed August 9, 2025, https://beckinstitute.org/about/dr-aaron-t-beck/
- Beck Depression Inventory (BDI) – American Psychological Association, accessed August 9, 2025, https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/beck-depression
- Assessment of depression in medical patients: A systematic review of the utility of the Beck Depression Inventory-II | Clinics – Elsevier, accessed August 9, 2025, https://www.elsevier.es/en-revista-clinics-22-articulo-assessment-depression-in-medical-patients-S1807593222016325
- Reliability and Validity of the Beck Depression Inventory-II among Korean Adolescents, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5240453/
- Beck Depression Inventory-Second Edition | The National Child Traumatic Stress Network, accessed August 9, 2025, https://www.nctsn.org/measures/beck-depression-inventory-second-edition
- What Is the Beck Depression Inventory and How Do I Use It? – Verywell Mind, accessed August 9, 2025, https://www.verywellmind.com/what-is-the-beck-depression-inventory-5294126
- Beck Depression Inventory-II (BDI-II) – American Thoracic Society, accessed August 9, 2025, https://www.thoracic.org/members/assemblies/assemblies/srn/questionaires/bdi-ii.php
- How is the Beck Depression Inventory Administered – MEDvidi, accessed August 9, 2025, https://medvidi.com/blog/what-is-the-beck-depression-inventory-and-how-to-use-it
- SciELO Brasil – Psychometric properties of the Beck Depression …, accessed August 9, 2025, https://www.scielo.br/j/rbp/a/84pk6g6z4FVyGtkncK4m6XR/?lang=en
- Psychometric properties of the Beck Depression Inventory-II: a comprehensive review, accessed August 9, 2025, https://www.scielo.br/j/rbp/a/84pk6g6z4FVyGtkncK4m6XR/abstract/?lang=en
- Psychometric Properties – Physiopedia, accessed August 9, 2025, https://www.physio-pedia.com/Psychometric_Properties
- Assessment of depression in medical patients: A systematic review of the utility of the Beck Depression Inventory-II – PMC, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3782729/
- Validity and reliability of the Beck Depression Inventory II (BDI-II) in family caregivers of children with chronic diseases | PLOS One, accessed August 9, 2025, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0206917
- (PDF) Depression as Measured by the Beck Depression Inventory-II Among Injecting Drug Users – ResearchGate, accessed August 9, 2025, https://www.researchgate.net/publication/7107485_Depression_as_Measured_by_the_Beck_Depression_Inventory-II_Among_Injecting_Drug_Users
- Psychometric Evaluation of the Beck Depression Inventory-II With Primary Care Medical Patients – ResearchGate, accessed August 9, 2025, https://www.researchgate.net/publication/230896347_Psychometric_Evaluation_of_the_Beck_Depression_Inventory-II_With_Primary_Care_Medical_Patients
- Measurement-based care – APA Services, accessed August 9, 2025, https://www.apaservices.org/practice/measurement-based-care
- Use of Measurement-Based Care for Behavioral Health Care in Community Settings – A Brief Report – SAMHSA, accessed August 9, 2025, https://www.samhsa.gov/sites/default/files/ismicc-measurement-based-care-report.pdf
- Implementing Measurement-Based Care for Depression: Practical Solutions for Psychiatrists and Primary Care Physicians, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7813452/
- Understanding psychological testing and assessment, accessed August 9, 2025, https://www.apa.org/topics/testing-assessment-measurement/understanding
- The Efficacy of Measurement-Based Care for Depressive Disorders: Systematic Review and Meta-Analysis of Randomized Controlled Trials – Psychiatrist.com, accessed August 9, 2025, https://www.psychiatrist.com/jcp/measurement-based-care-depression/
- Reviewing the Beck Depression Inventory on Its Psychometric Properties – ResearchGate, accessed August 9, 2025, https://www.researchgate.net/publication/392626911_Reviewing_the_Beck_Depression_Inventory_on_Its_Psychometric_Properties
- What Is The Beck Depression Inventory In Mental Health? – BetterHelp, accessed August 9, 2025, https://www.betterhelp.com/advice/depression/what-is-the-beck-depression-inventory/
- Measurement-Based Care for the Treatment of Depression – Psychiatric Times, accessed August 9, 2025, https://www.psychiatrictimes.com/view/measurement-based-care-treatment-depression
- Self-Report Bias and Underreporting of Depression on the BDI-II – ResearchGate, accessed August 9, 2025, https://www.researchgate.net/publication/10902923_Self-Report_Bias_and_Underreporting_of_Depression_on_the_BDI-II
- The Beck Depression Inventory (BDI-II) and a single screening question as screening tools for depressive disorder in Dutch advanced cancer patients, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3244603/
- (PDF) Cross-cultural comparison of depressive symptoms on the Beck Depression Inventory-II, across six population samples – ResearchGate, accessed August 9, 2025, https://www.researchgate.net/publication/358524575_Cross-cultural_comparison_of_depressive_symptoms_on_the_Beck_Depression_Inventory-II_across_six_population_samples
- Cross-cultural comparison of depressive symptoms on the Beck Depression Inventory-II, across six population samples, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8867877/
- Psychometric Properties and Cross-Cultural Invariance of the Beck Depression Inventory-II and Beck Anxiety Inventory among a Representative Sample of Spanish, Portuguese, and Brazilian Undergraduate Students – ResearchGate, accessed August 9, 2025, https://www.researchgate.net/publication/371199017_Psychometric_Properties_and_Cross-Cultural_Invariance_of_the_Beck_Depression_Inventory-II_and_Beck_Anxiety_Inventory_among_a_Representative_Sample_of_Spanish_Portuguese_and_Brazilian_Undergraduate_Stu
- Beck Depression Inventory-II: Factor Analyses with Three Groups of Midlife Women of African Descent in the Midwest, the South, and the U.S. Virgin Islands – PMC – PubMed Central, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5889520/
- BDI®-II | Beck Depression Inventory® – Second Edition described in ePROVIDE, accessed August 9, 2025, https://eprovide.mapi-trust.org/instruments/beck-depression-inventory-r-second-edition
- BDI–II – Beck Depression Inventory-II | Pearson Clinical Assessment …, accessed August 9, 2025, https://www.pearsonclinical.ca/en-ca/Store/Professional-Assessments/Personality-%26-Biopsychosocial/Brief/Beck-Depression-Inventory-II/p/P100008037
- Read the Belmont Report | HHS.gov, accessed August 9, 2025, https://www.hhs.gov/ohrp/regulations-and-policy/belmont-report/read-the-belmont-report/index.html
- Ethical Issues and Challenges Regarding the Use of Mental Health Questionnaires in Public Health Nutrition Research – PMC, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11858303/
- Screening for depression in medical research: ethical challenges …, accessed August 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3556128/
- Beck depression inventory scoring guide, accessed August 9, 2025, https://cdn.prod.website-files.com/66f3d5c1804bde949975d01a/67182b7b309eff923d9414de_gukitenutakatibutonoret.pdf